
Prior Authorization Specialist - Drive Exceptional Patient Care With Precision and Accuracy
Employer
Vitreoretinal Surgery PLLC
Salary
$55k-$65k (estimated pay)
Location
Minneapolis, MN
Employment Type
Full-time
Сategory
Medical Assistants
Description
Passionate about patient care and prior authorizations? Join our team as a Prior Authorization Specialist at Vitreoretinal Surgery PLLC in Edina, MN!
Qualifications
- medical insurance experience
- strong computer experience
- problem solving skills
Responsibilities
- coordinate prior authorization requests
- follow up on prior authorization requests
- review approved prior authorizations
Education
One year experience with appeal submissions and/or medical billing and coding certificate strongly preferred
Working Hours
8am-5pm, Monday-Friday
Benefits
- Paid Holidays
- Health Insurance
- Dental Insurance
- Vision Insurance
Apply to this job
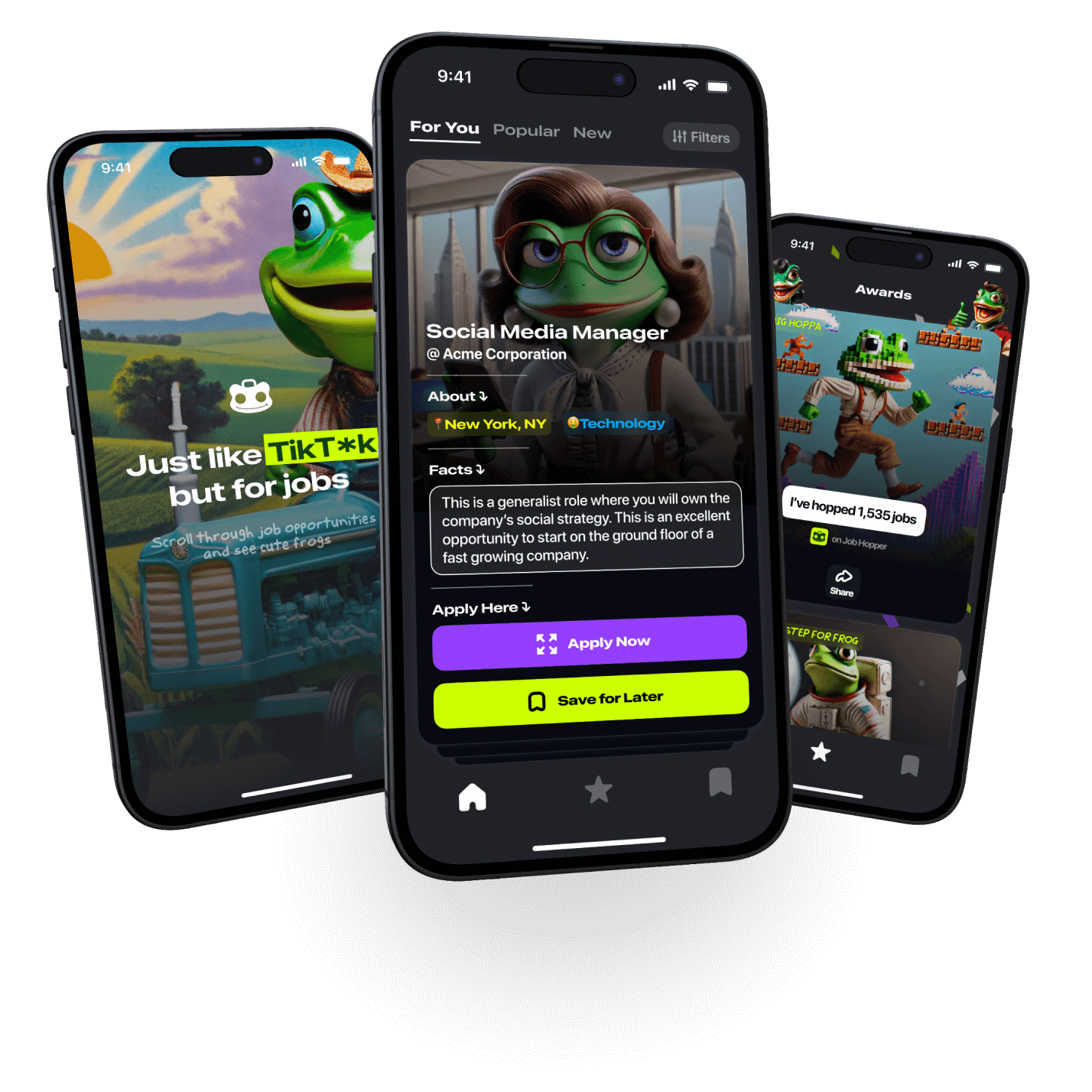
on Job Hopper

By entering your phone number, you agree
to Job Hopper’s Terms of Service


