
Claims Reviewer – Make a Real Impact in Claims Processing
Employer
TEEMA
Salary
$70k-$90k (estimated pay)
Location
Phoenix, AZ
Employment Type
Full-time
Сategory
Health Technicians
Description
Exciting opportunity for a detail-oriented Claims Reviewer to join a dynamic team and make a real difference in claims processing!
Qualifications
- High School Diploma or GED
- 2+ years of experience in medical claims review
Responsibilities
- Conduct retrospective review of medical, surgical, and behavioral health claims
- Evaluate claims for medical necessity and appropriateness
Keywords
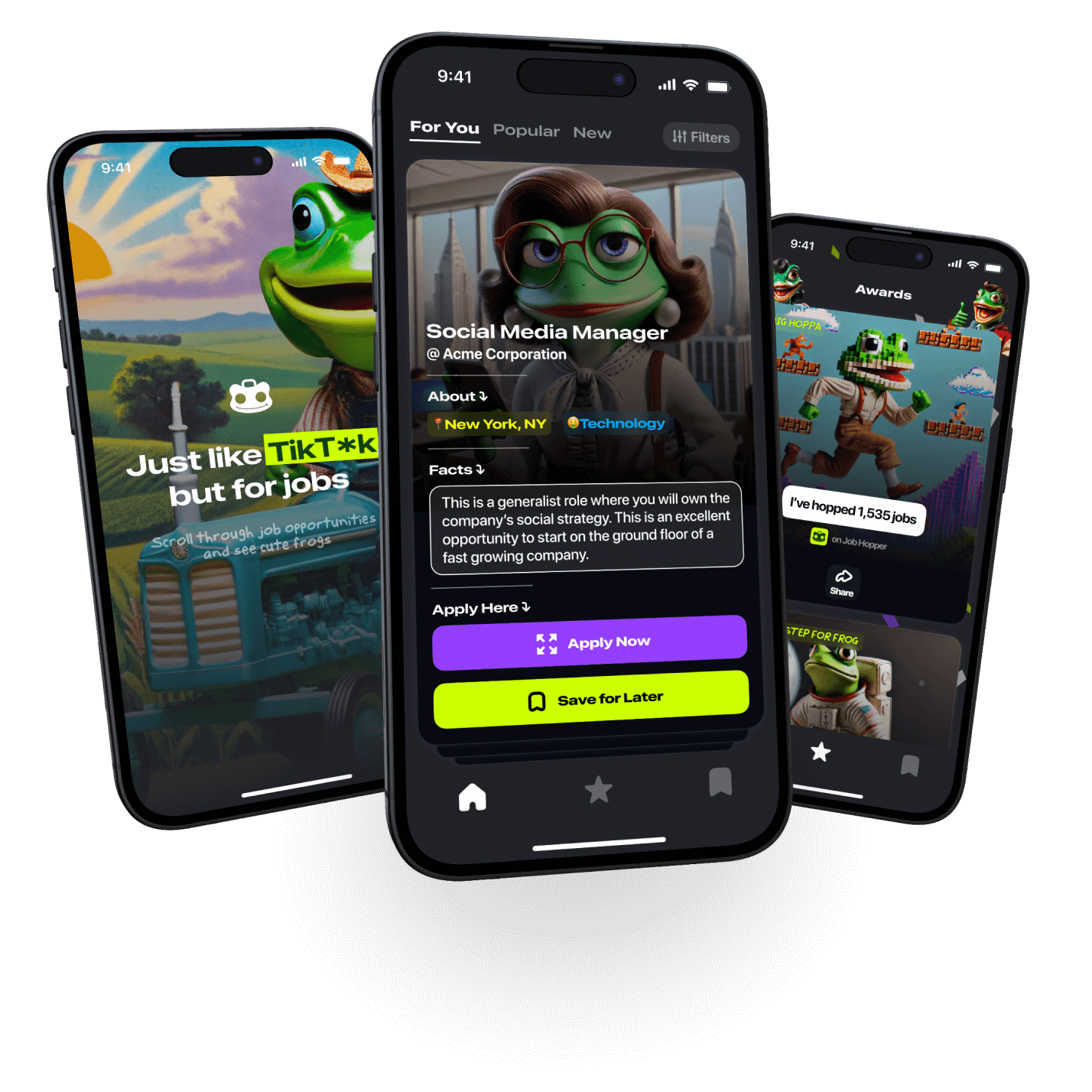
Apply to this job
on Job Hopper

By entering your phone number, you agree
to Job Hopper’s Terms of Service


