
Managed Care Claims Validator / Biller - Transforming Healthcare Billing Accuracy and Timeliness
Employer
CommuniCare Family of Companies
Salary
$50k-$70k (estimated pay)
Location
Akron, OH
Employment Type
Full-time
Сategory
Health Technicians
Description
Exciting opportunity at CommuniCare Family of Companies for a Managed Care Claims Validator / Biller. Join our team and ensure accurate and timely filing of managed care claims!
Qualifications
- High School graduate or GED required
- Prior work/life experience in a long term care setting preferred
Responsibilities
- Validate managed care claims for accuracy and timeliness
- Check and resolve claim rejections
- Identify trends in claim denials for review
Benefits
- Competitive wages
- Paid time off
- Benefit options including medical, dental, and vision coverage
- 401(k) with employer match
- Flexible spending accounts
Apply to this job
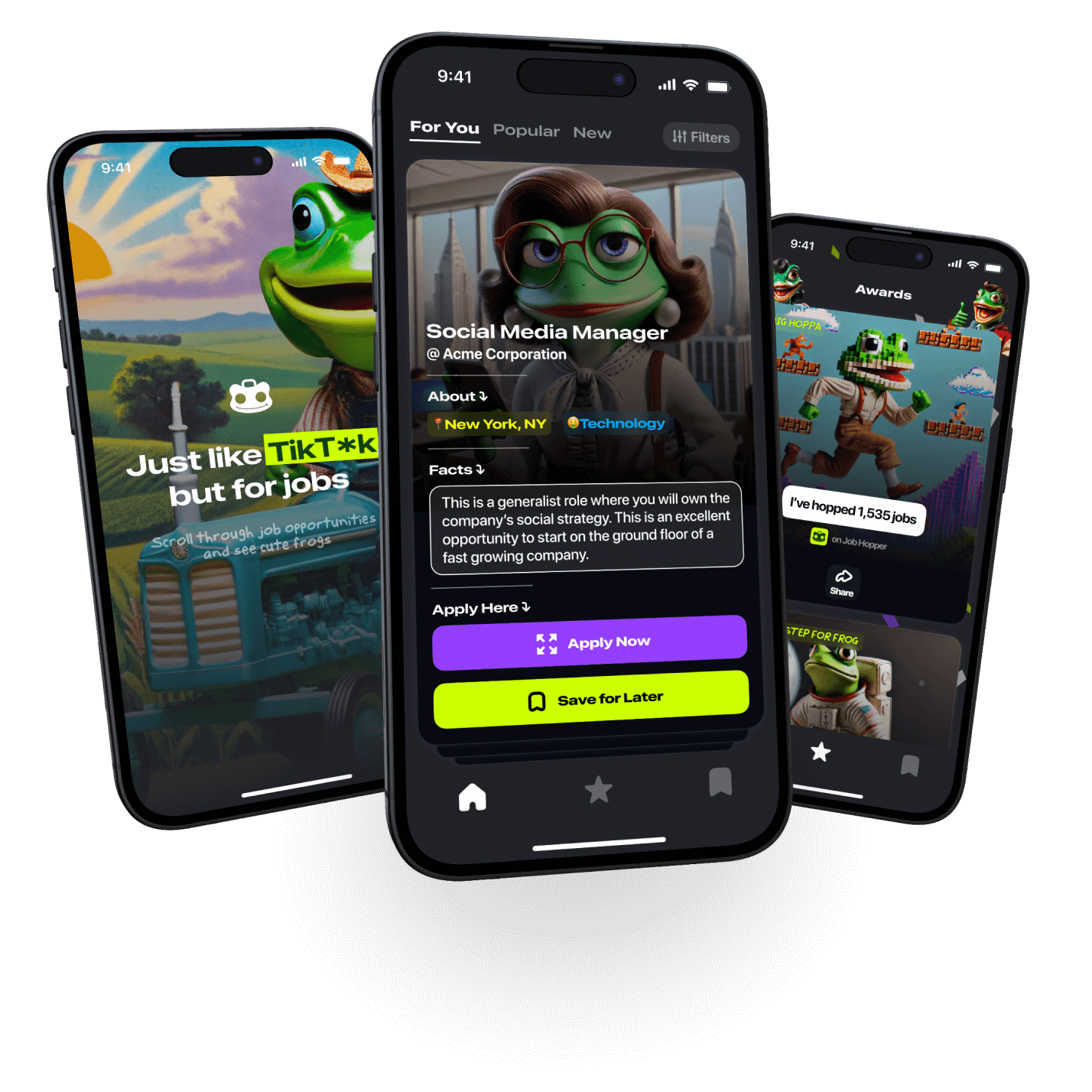
on Job Hopper

By entering your phone number, you agree
to Job Hopper’s Terms of Service


